GME and Economic Development: Why It Matters
Written By: Vance Farrow, Healthcare Industry Specialist
Nevada is at a crossroads. Rapid population growth, uneven access to care across urban and rural communities, and a tight physician workforce threaten both the health of Nevada’s residents and the economic momentum of the state. Expanding Graduate Medical Education (GME) – the residency and fellowship training that medical school graduates complete to become practicing physicians is one of the highest-leverage, evidence-backed strategies Nevada can deploy to strengthen health outcomes and drive sustained economic development.
What Is GME?
Graduate Medical Education refers to the accredited residency and fellowship programs where newly minted physicians receive supervised clinical training. That training determines not only specialty and clinical competence, but it also strongly influences where doctors ultimately practice. Nationwide, doctors who complete residency programs in a state are far more likely to stay and practice there, especially for primary care and other shortage specialties. For Nevada, which has long lagged other states in per-capita physician supply and still faces many primary care and rural shortage areas, keeping more trainees local is a direct pathway to closing access gaps. Nevada nationally ranks 6th in the percentage of GME graduates (55.2%) who choose to remain local to practice. Additionally, Nevada ranks nationally 8th in the percentage (76.9%) of physicians who attended Nevada undergraduate and graduate medical education and chose to remain local to practice. (AAMC, 2023).
But the benefits of GME are not purely clinical. Residency programs create high-wage jobs (physicians, nurse educators, program coordinators), drive research and philanthropy, boost hospital and clinic revenues, and generate downstream economic activity (housing, retail, professional services). Analyses of other states’ GME expansions demonstrate measurable increases in local economic output, job creation, and tax revenue, making GME a clear economic development instrument, not just health workforce policy.
We Are Making Progress – But Still a Gap
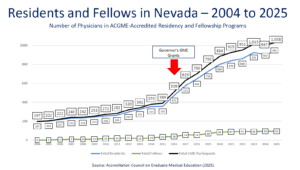
Nevada has made important progress. Nevada’s medical schools and health systems have added programs and slots over the past two decades, and the number of physicians completing ACGME-accredited programs in the state rose substantially between 2004 and 2024. However, demand has outpaced supply. Large parts of rural Nevada and many urban neighborhoods remain designated Health Professional Shortage Areas (HPSAs) for primary care and mental health, and Nevada continues to recruit many of its physicians from outside the state. That dynamic leaves long wait times, care deserts, and avoidable reliance on emergency care — all of which have direct economic costs through lost productivity and higher healthcare spending.
There have been seven previous rounds of state-sponsored GME funding, creating additional residency programs in a variety of areas, including primary care, Psychiatry, OB/GYN, Surgery, Geriatric Medicine, and many others. At the same time, Nevada has shown it can make structural changes happen. Investments like the Kirk Kerkorian School of Medicine and the newly accredited Roseman University College of Medicine reflect a growing consensus that Nevada must own its physician workforce pipeline. These investments create the institutional capacity to host more residents, but capacity needs funding, clinical training sites, faculty, and system coordination to scale effectively.
How GME Expansion Creates Economic Value
- Direct employment and payroll: Residents and faculty are employees who spend locally. Hospitals that host residency programs hire additional educators, coordinators, and administrative staff. Those jobs are often well-paid and stable, raising household incomes and consumer spending.
- Clinical revenue and system efficiency: Teaching programs tend to broaden the range of services hospitals and clinics can offer (e.g., specialty clinics, complex procedures, behavioral health integration). That increases revenue, attracts referrals, and enables health systems to retain patient dollars that would otherwise go out of state.
- Attraction and retention of physicians: Each additional residency slot yields a higher probability that a physician will remain in state after training, especially if tied to community-based rotations in rural areas. Those retained physicians deliver ongoing economic value.they run practices, employ staff, and stabilize care access.
- Research, innovation, and commercialization: Academic clinical programs attract research grants, clinical trials, and partnerships with biotech and life sciences firms. Over time, these create cluster effects; clinics, labs, startups, and service firms gravitate toward a robust medical education ecosystem.
- Tax base and multiplier effects: Studies of other states show that GME investments generate multipliers across the economy (supplier purchases, construction for facilities, increased consumer spending), producing net gains in state GDP and tax receipts. Tripp Umbach, Mathematica, and other independent analyses consistently show sizable returns when states strategically expand GME.
Evidence From Other States (What Nevada Has Learned)
When states have intentionally funded residency expansion, the results are tangible. For example, economic impact assessments in multiple states show that adding residency positions leads to meaningful increases in employment, hospital capacity, and long-term physician retention. Those assessments typically account for direct payroll, indirect supplier effects, and induced household spending.They consistently show that GME programs are a cost-effective way to build human capital and regional economic resilience. Nevada can follow best practices, target primary care and shortage specialties, incentivize rural rotations, and link funding to demonstrated retention outcomes.
What’s Next…

During the 2023 Legislative Session, the Nevada Legislature passed SB350, which statutorily established the GME Advisory Council and Grant Program. After that, during the most recent 2025 Legislative Session, the Nevada Legislature passed SB262 and SB494, revising the GME Grant Program and Advisory Council, and transferring authority from the Office of Science, Innovation, and Technology to the newly created Nevada Health Authority. Members of the GME Advisory Council have been appointed by the Governor’s Office, and we have already begun the planning phase for the eighth round of GME funding.
Investing in GME is not a short-term bailout for healthcare access. It is infrastructure building, human infrastructure. Just as roads, ports, and broadband are long-lived investments that enable commerce, a state’s ability to train, employ, and retain physicians is an enduring foundation for community health, business recruitment, and resilience. For Nevada, a state that has demonstrated it can mobilize resources for transformative projects, prioritizing and scaling GME is one of the smartest bets it can make to ensure health equity and dynamic economic development in healthcare for decades to come.


